Treatments
Arterial Disease
Peripheral Arterial Interventions
Angiogram
A peripheral angiogram, also known as an extremity angiogram, is a minimally invasive imaging test that uses X-rays and dye to examine the arteries in the arms, hands, legs, or feet. The test can help doctors detect blood flow issues and narrowed arteries, which can increase the risk of heart attack or stroke.

During the procedure, a patient will:
After the procedure, patients should avoid driving or operating equipment for the first 24 hours, but they can walk around the house and do light activity.
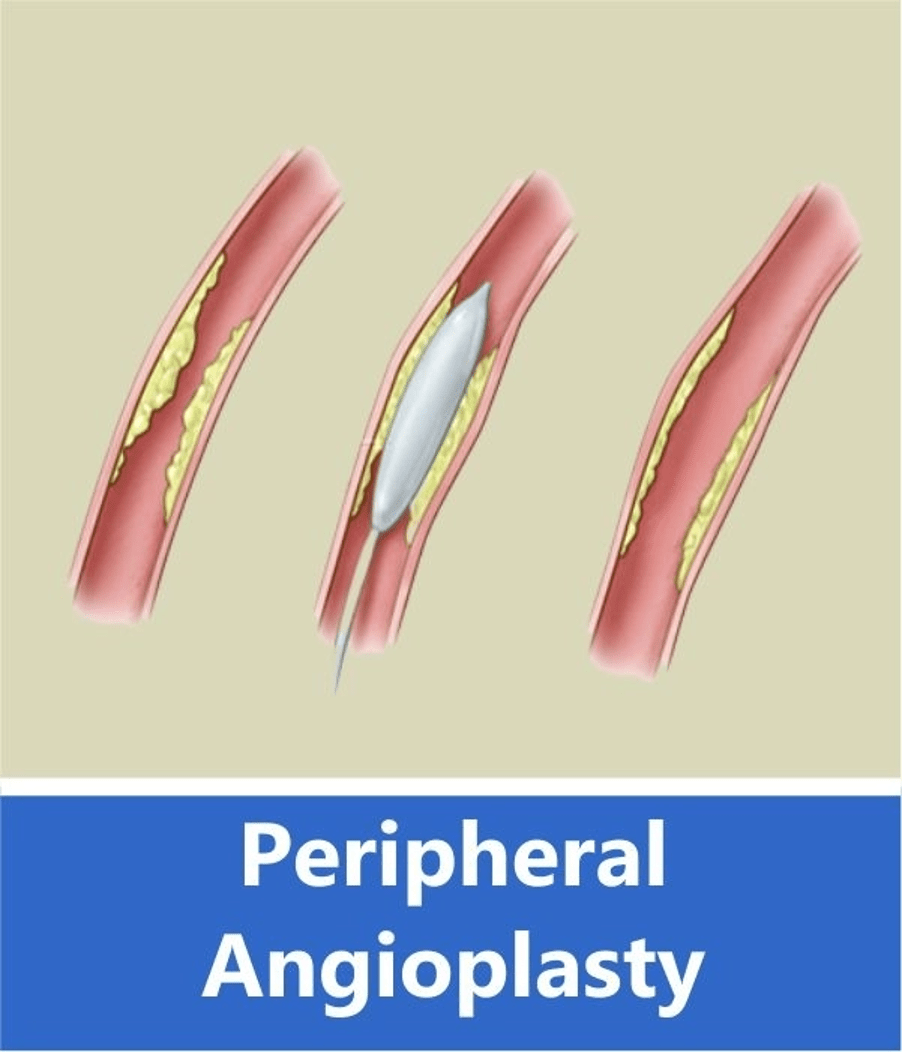
Angioplasty
Peripheral angioplasty (PAA) is a minimally invasive procedure that uses a catheter and balloon to open blocked arteries in the extremities, such as the arms or legs. The procedure can help improve blood flow, reduce leg pain, and help wounds heal better. It can also help patients walk farther without leg pain.
A doctor may recommend PAA if a patient has peripheral artery disease (PAD), which can cause symptoms such as: Chronic leg pain, Heavy feeling in the legs, Limitations to daily activities, and Wounds on the legs or feet that don’t heal.
During the procedure, a patient is awake and receives medicine to help them relax and prevent pain. A doctor then inserts a catheter into an artery in the groin or leg and guides it through to the peripheral artery using X-ray equipment. The balloon is then pressed against the inside wall of the artery to open the space and improve blood flow.
Risks of PAA include:
It can take 6 to 8 weeks to fully recover from PAA, and the leg on the side of the procedure may be swollen for a few days or weeks.
To prepare for the procedure, patients should:
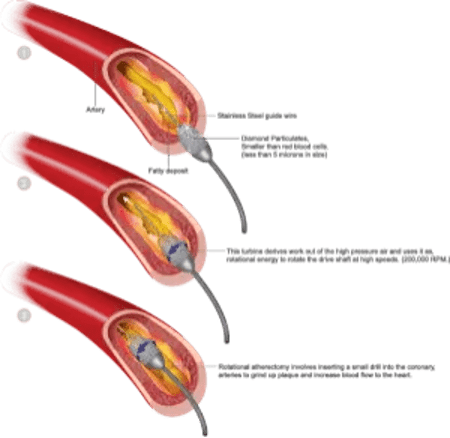
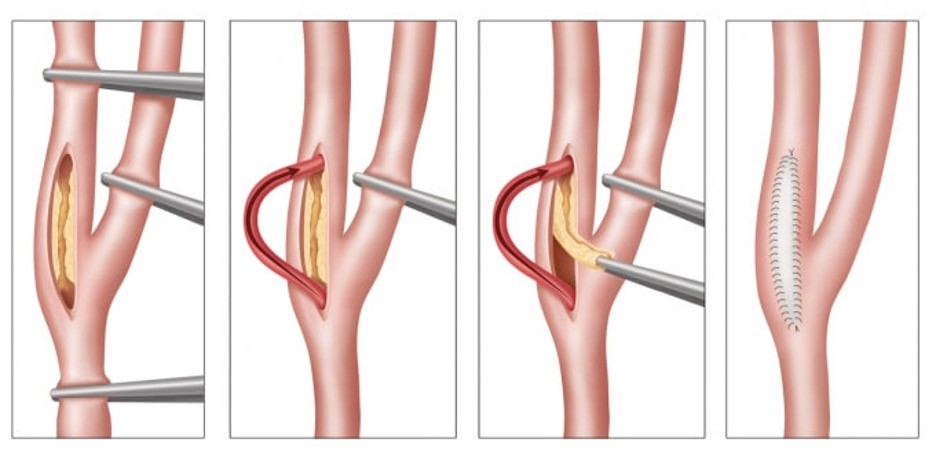
Atherectomy
Peripheral atherectomy is a minimally invasive procedure that removes plaque from arteries to restore blood flow. It’s a peripheral intervention that’s especially effective for people with peripheral artery disease (PAD), which occurs when plaque builds up in the arteries that supply blood to the limbs, organs, and head. The plaque, also known as atherosclerosis, can narrow the arteries and reduce blood flow.
Peripheral atherectomy is a minimally invasive procedure that removes plaque from arteries to restore blood flow. It’s a peripheral intervention that’s especially effective for people with peripheral artery disease (PAD), which occurs when plaque builds up in the arteries that supply blood to the limbs, organs, and head. The plaque, also known as atherosclerosis, can narrow the arteries and reduce blood flow.
During a peripheral atherectomy, a healthcare provider uses a catheter with a sharp blade, laser, or rotating device on the end to scrape away, dissolve, or break up the plaque. The type of technique used depends on the extent of the plaque buildup. For example, peripheral laser atherectomy uses a catheter that emits high-energy light to vaporize the blockage.
A doctor may recommend atherectomy if:
Bypass
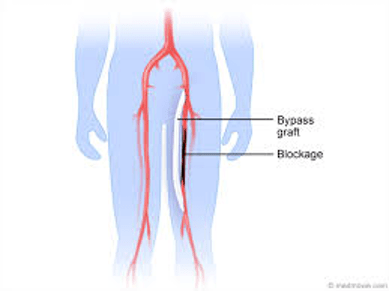
Peripheral arterial bypass grafting, also known as peripheral vascular bypass or lower extremity bypass, is a surgical procedure that reroutes blood flow around a blocked artery in the leg. The procedure uses a graft, which is a special tube that replaces the blocked part of the artery. Grafts can be made from natural human tissue or synthetic materials like Dacron or polytetrafluoroethylene (PTFE). The graft is often a vein taken from another part of the leg, but can also be a man-made blood vessel.
During the procedure, the surgeon makes an incision over the blocked artery, usually in the leg, groin, or lower belly. Clamps are placed on either end of the blocked section, and the graft is sewn into the artery to create a new pathway for blood flow. Before closing the incision, the surgeon will check to make sure blood is flowing through the graft correctly.
After surgery, patients typically stay in the hospital for a few days to a week. They may need to spend 1–3 days in the intensive care unit (ICU) before moving to a regular hospital room. During recovery, patients may experience mild pain and swelling at the incision site, as well as fatigue for a few weeks to a month. Their doctor may recommend physical therapy, and patients should arrange for someone to drive them home from the hospital. Once home, patients may need help with everyday tasks for a week or more, and should avoid strenuous activities for as long as their doctor recommends. It’s also important to keep the incision area clean and change the surgical dressing frequently to prevent infection.
After the blood flow is restored, symptoms usually improve or go away completely. However, it’s important to maintain a healthy lifestyle to prevent future blockages. Patients should contact their provider if they experience any of the following problems after going home: Fever or chills, something coming out of the incisions, and any change in how the leg looks or feels.
Stenting
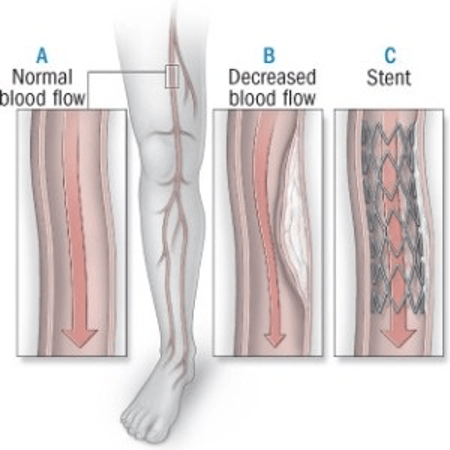
Peripheral Angioplasty and Stenting. Angioplasty is a procedure that uses a catheter and a balloon to open up blocked arteries. Stenting happens after angioplasty during which your surgeon inserts a small metal device in the artery. The stent helps keep the artery open and improve blood flow.
During the procedure, a doctor inserts a flexible tube, called a catheter, into the artery through a cut in the groin and uses X-rays to guide it to the blockage. The stent is then passed through the catheter and implanted into the artery, where it remains permanently. Stenting is often performed in conjunction with angioplasty, a procedure that uses a balloon catheter to open the artery.
After the procedure, most people can go home from the hospital in two days or less and should be able to walk around within 6 to 8 hours. Your provider will explain how to take care of yourself.
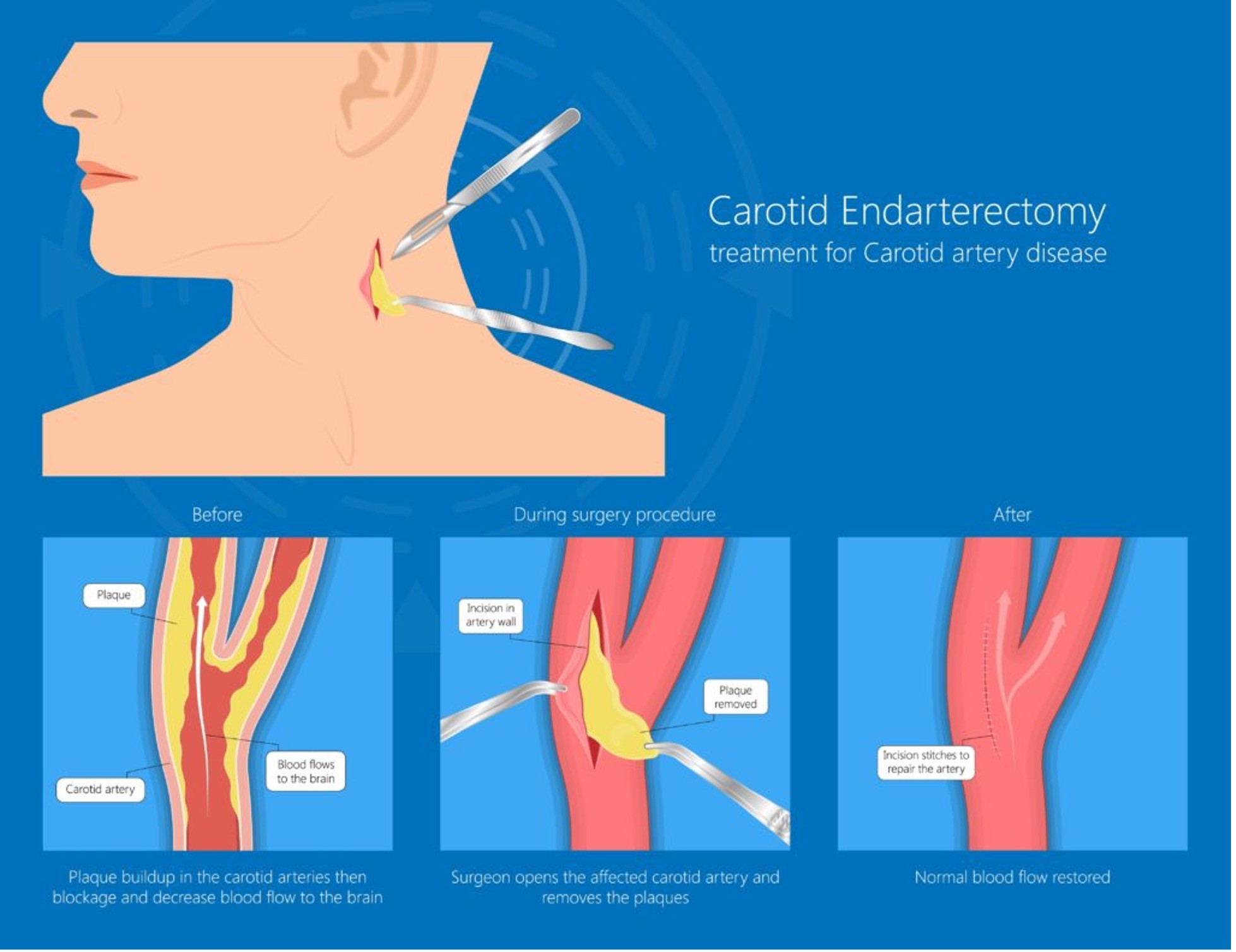
Carotid Endarterectomy
Carotid endarterectomy (CEA) is a surgical procedure that reduces the risk of stroke by removing plaque from the carotid arteries. The carotid arteries are the main blood vessels that supply blood to the brain, face, and neck. When plaque, a fatty substance, builds up in the carotid arteries, it can narrow them and reduce blood flow to the brain, which can increase the risk of stroke.
During a CEA, a surgeon makes an incision in the neck over the affected carotid artery, opens the artery, and removes the plaque. The surgeon may also leave a small tube in the wound to drain any blood that builds up after the operation. After the procedure, patients are usually moved to the recovery area to be monitored.
Most patients can return to normal activities within 3 to 4 weeks, but may experience a slight neck ache for about 2 weeks. They may also need help with meals, shopping, and other tasks at first.
The two main risks of a CEA are stroke and death. The risk of stroke is around 2%, but may be higher for people who have had a stroke before the operation. The risk of death is less than 1%, and can occur as a result of complications such as a stroke or heart attack.
Transcarotid Arterial Revascularization (TCAR)
Transcarotid artery revascularization (TCAR) is a minimally invasive surgical procedure that treats carotid artery disease (carotid stenosis) and prevents strokes:
TCAR is designed to minimize the risk of stroke by keeping potential stroke-causing fragments away from the brain. Patients typically spend just one night in the hospital and recover quickly. Before leaving the hospital, a doctor will provide advice for activity, diet, and medications. Patients will be asked to avoid hard activities like lifting for at least a week and will be told when they can resume normal activity and return to work. Doctors will also prescribe medications to prevent blood clots from forming in the newly opened artery.
TCAR can be performed under either general anesthesia or MAC, with the anesthetic technique based on neck anatomy and the patient’s ability to tolerate lying still.
Endovascular Aortic Aneurysm Repair (EVAR)
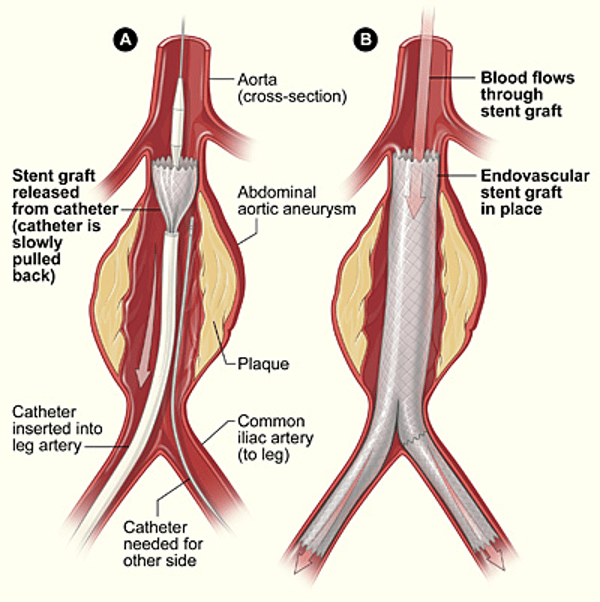
Endovascular aneurysm repair (EVAR) is a minimally invasive procedure to treat an abdominal aortic aneurysm (AAA) from the inside of the aorta, the body’s largest artery:
EVAR can help relieve pressure on the aneurysm and prevent it from rupturing. Benefits of the procedure include a faster recovery, shorter hospital stay, and less pain after surgery. However, there are some risks associated with EVAR, including:
After the procedure, patients are usually sedated and monitored for heart rate, blood pressure, breathing, and blood oxygen level. They may also receive medication to help them relax and for pain relief. Many people can go home the next day and return to their normal activities, but they should avoid rigorous exercise and heavy lifting for two weeks
Open Abdominal Aortic Aneurysm Repair
Open abdominal aortic aneurysm (AAA) repair is a major surgical procedure that involves replacing a widened section of the aorta with a synthetic graft:
Open AAA repair is a safe and effective procedure that can prevent aneurysm rupture and has a good long-term outlook. However, there is a risk of complications, including heart attack, stroke, kidney failure, and infection. The procedure usually takes about three hours and patients typically stay in the hospital for 7–14 days, spending some time in the intensive care unit. It can take several months to return to normal activities and work.
Joint Pain
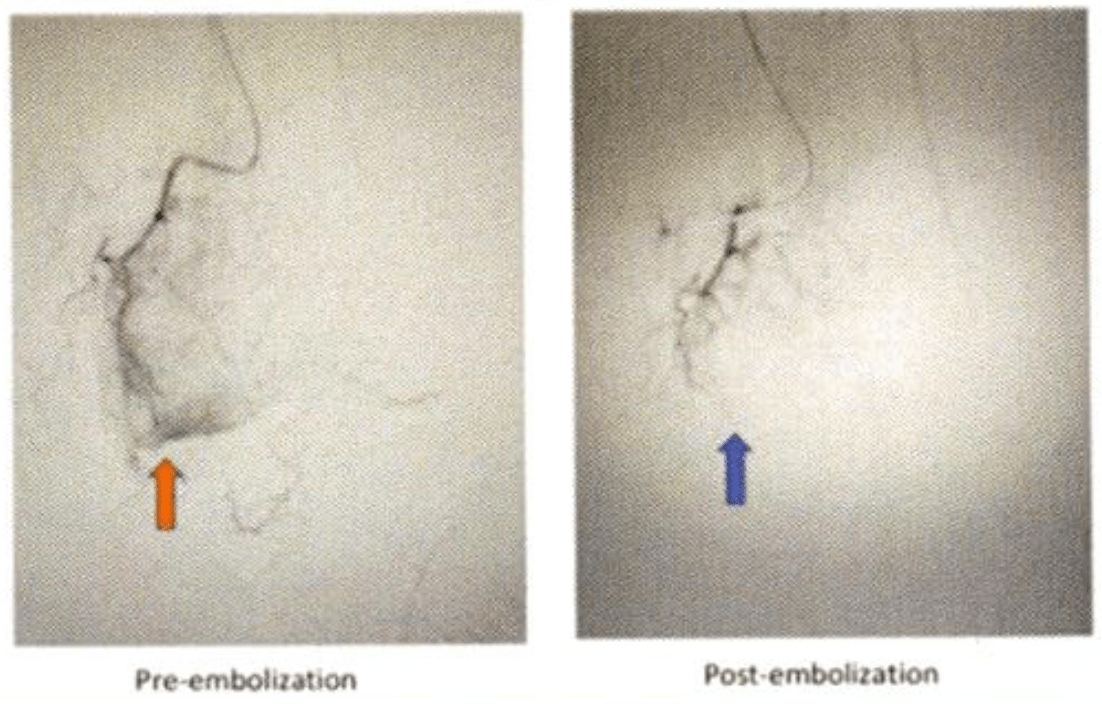
Genicular Artery Embolization
Genicular artery embolization (GAE) is a minimally invasive procedure that can treat knee pain caused by osteoarthritis (OA) and recurrent hemarthrosis after total knee arthroplasty (TKA). GAE reduces blood flow to the knee’s lining, or synovium, by blocking abnormal blood vessels caused by arthritis. This can help or eliminate knee pain.
Kidney Disease and Dialysis Access
AV Fistulogram
A fistulogram is a type of X-ray. It uses X-ray dye (contrast) to look inside your arteriovenous (AV) fistula vascular access for hemodialysis. It’s done to check the blood flow and look for any narrowing (stenosis) in the vein of your fistula. If a narrowing is found, then an angioplasty can be done at the same time. This procedure widens the vein using a small, inflatable balloon. Fistulogram and angioplasty are both outpatient procedures. This means you’ll go home the same day.
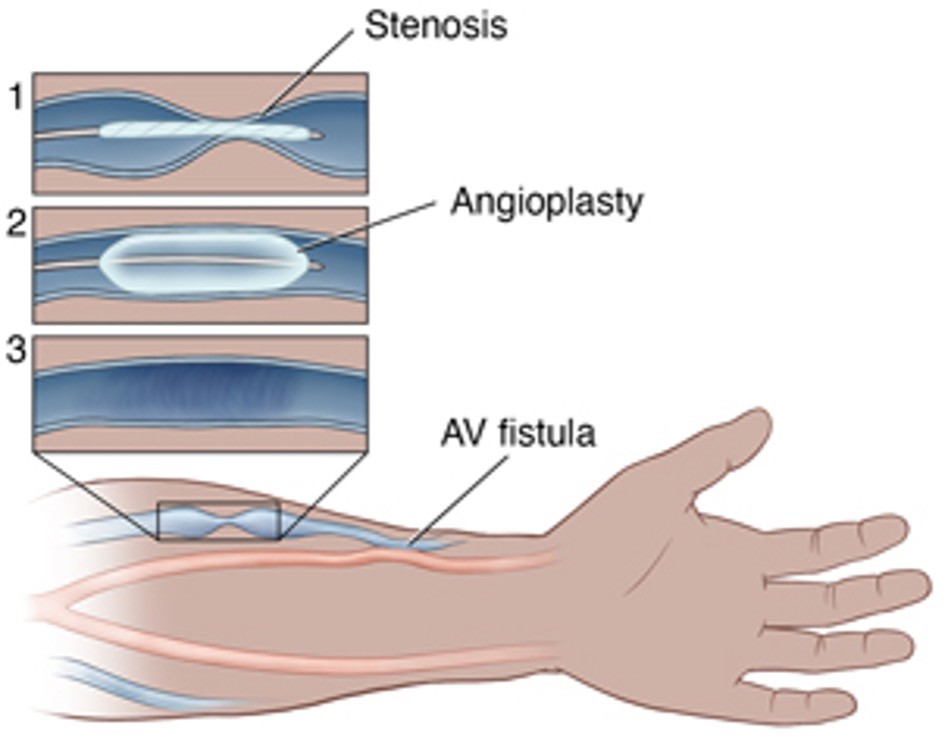
Why is a fistulogram and/or angioplasty done?
This procedure may be advised if you have any signs that your AV fistula isn’t working well due to a narrowed blood vessel. This can include:
Before the procedure
During the procedure
In general, here’s what you can expect during a fistulogram and angioplasty:
If an angioplasty is needed:
After the procedure
Risks of fistulogram and angioplasty
All procedures have some risk. Possible risks of fistulogram and angioplasty are:
When to call your healthcare provider
Call your healthcare provider if any of these occur after the procedure:
Tunneled Dialysis Catheter Placement
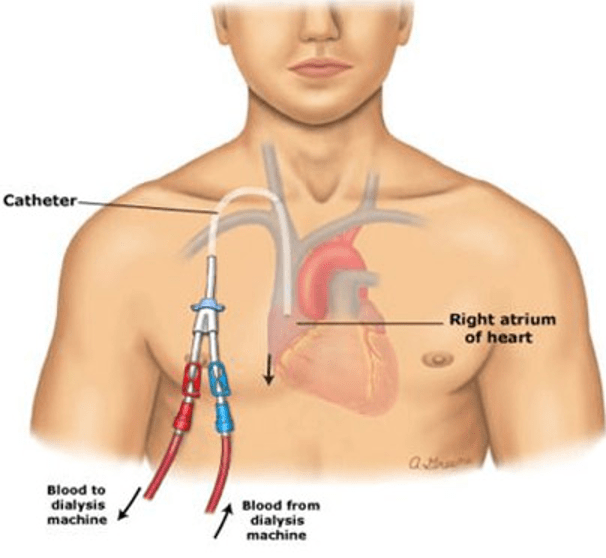
A permcath, or tunneled hemodialysis catheter, is a soft plastic tube that’s surgically inserted into a vein in the neck or groin for short-term dialysis treatment:
The procedure can take about 45 minutes and may involve blood tests, a physical examination, a Doppler scan, IV cannula, sedatives, and X-ray imaging tests. The area is numbed with general anesthetic or lidocaine. After the permcath is in place, it’s important to take proper care of it to avoid infections and complications, such as migration. Signs of infection include redness and swelling.
A permcath can remain in place for up to 12 months, but it may need to be replaced if an infection occurs. A permcath may be necessary if a fistula or graft formation is not possible or appropriate, or if the kidneys aren’t working well enough to remove toxins and fluid from the body
Dialysis Catheter Removal/Exchange
Catheter exchange is a procedure that can help extend the life of a permacath, or tunneled hemodialysis catheter. A permacath is a flexible plastic tube that’s surgically attached to a vein in the neck or chest and threaded to the right side of the heart. It has two tubes inside, one to carry blood to a dialysis machine and the other to return blood to the patient. The catheter can remain in place for up to 12 months.
Declot Procedure
A declot procedure, also known as a thrombectomy, is a mechanical method to remove a blood clot from an artery or vein. It’s often performed to improve blood flow in arteriovenous fistulae (AVFs) and grafts, which are used for dialysis. A declot can help clear blockages that may interfere with dialysis treatment
During a declot procedure, a specialist may use a catheter to break up the clot or a balloon to widen the vessel. For example, a small balloon can be inserted into the clot and then pulled out through a straw-like sheath. Other devices may also be used to help dissolve and remove the clot. To prevent the access from clotting again during the procedure, patients often receive blood thinners, heparin, or TPA. They may also receive medication to help them feel comfortable during the procedure.
A declot procedure can range in complexity and time, and it’s important to have a responsible adult to drive you home after the procedure. You should be able to resume your normal activities, including driving, after 24 hours, but you should avoid strenuous activity, exercising, or lifting heavy objects for that time.
Common complications of a declot procedure include bleeding, an allergy to x-ray dye, and a slight risk of infection. In rare cases, a piece of the clot could break off and travel to your lungs or hand, which may require further treatment
AV Fistula/Graft Creation
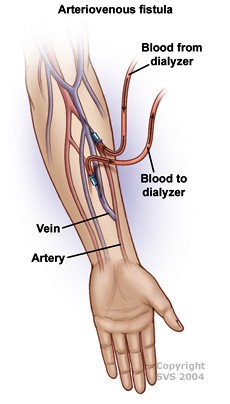
An arteriovenous (AV) fistula is a surgical procedure that creates a connection between an artery and a vein in the arm or leg to provide access for a dialysis machine. A vascular surgeon performs the procedure, which is usually done under general anesthetic in a hospital. The patient can typically go home the same day or a few hours after the procedure.
After the procedure, patients should avoid driving or operating machinery for the first 24 hours. They should also avoid heavy lifting or carrying heavy bags until they have regained full movement of their arm.
Arteriovenous Graft
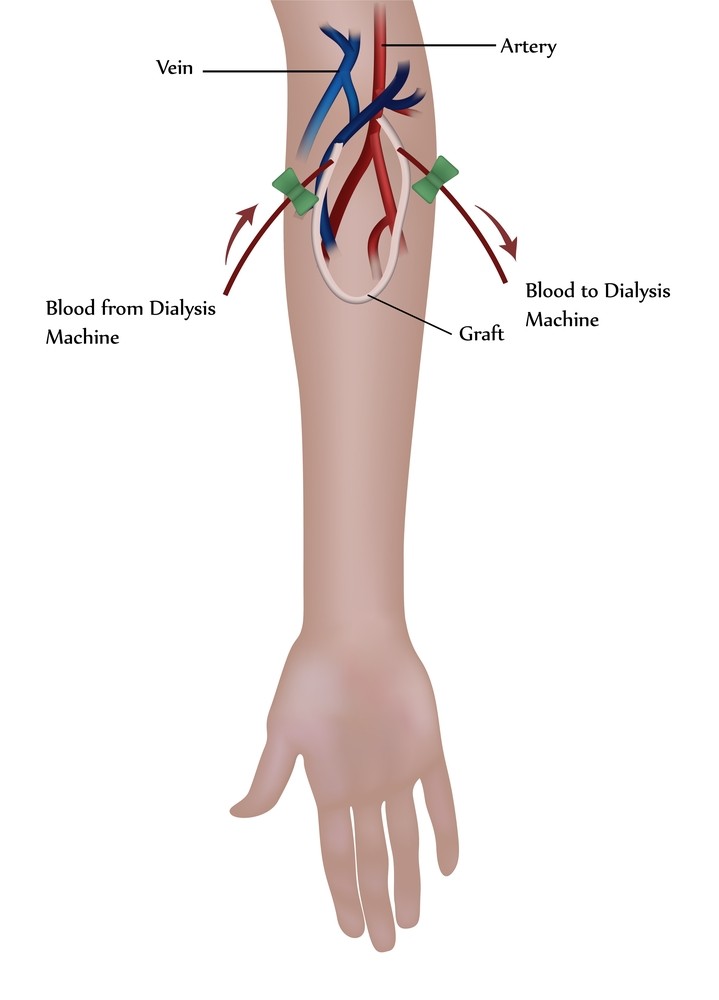
An arteriovenous (AV) graft is a surgical procedure that creates a looped plastic tube that connects an artery to a vein. A vascular surgeon performs the procedure in a hospital or outpatient center using local anesthesia to numb the area.
Renovascular Angioplasty and Stenting
Renal artery angioplasty and stenting is a minimally invasive procedure that treats narrowed renal arteries, the main blood vessels that supply blood to the kidneys:
This procedure can increase blood flow to the kidneys and lower blood pressure. It’s often the first procedure used for people with renal artery stenosis because it involves less recovery time than conventional surgery.
Some conditions that may contraindicate renal artery angioplasty and stenting include:
Venous Disease
IVC Filter Placement
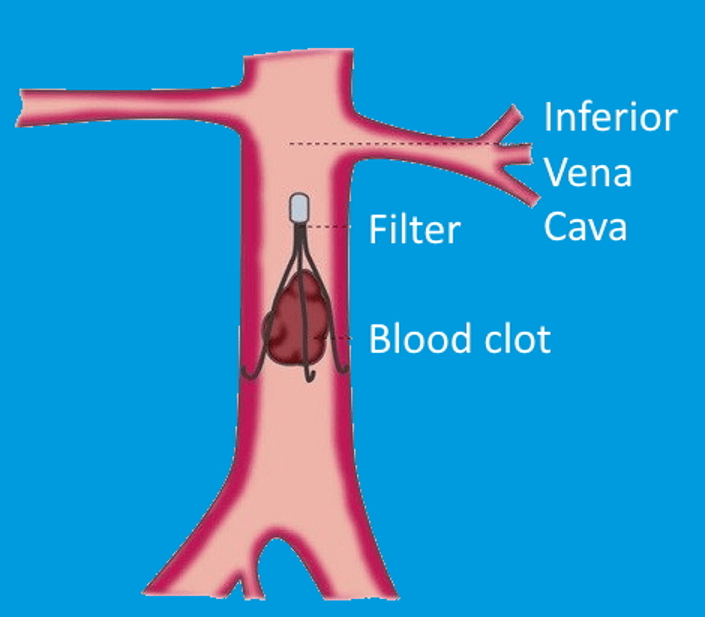
Inferior vena cava (IVC) filter placement is a procedure that involves inserting a filter into the inferior vena cava (IVC) to prevent blood clots from reaching the heart and lungs. The procedure is usually completed within an hour and most patients can go home the same day.
IVC Filter Removal
An interventional radiologist (IR) physician can remove an inferior vena cava (IVC) filter using a procedure similar to the one used to place it:
Venoplasty
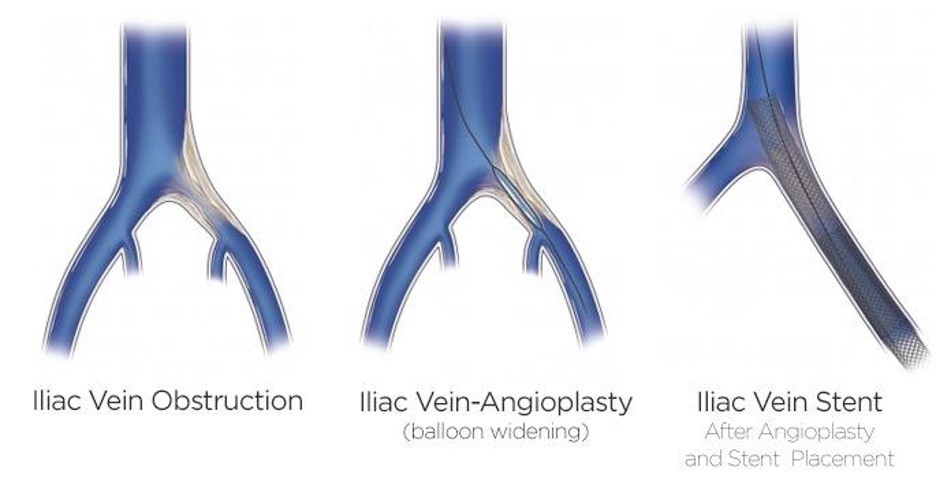
Venoplasty, also known as venous angioplasty, is a minimally invasive procedure that treats blocked or narrowed veins. It’s performed by doctors who specialize in interventional radiology.
Venoplasty can be used to treat deep venous disease, also known as iliac compression syndrome or May Thurner syndrome. It can also be used to create a temporary entry point for placing additional leads in heart rhythm procedures.
Benefits of venoplasty include:
Laser Ablation
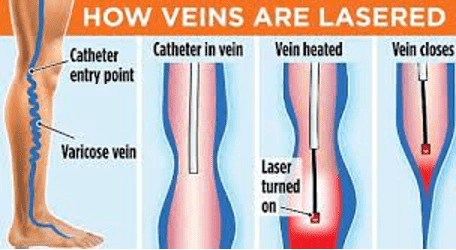
Endovenous laser ablation (EVLA) is a minimally invasive procedure that uses a laser to treat varicose veins. The procedure involves inserting a laser fiber into the vein through a small incision, numbing the area with local anesthetic, and then slowly withdrawing the catheter while activating the laser. The laser’s light energy heats the surrounding tissue, damaging the vein wall and causing it to collapse and turn into scar tissue. This allows healthy veins to resume normal blood flow.
EVLA is considered an effective treatment for varicose veins, with a reported success rate of 95–98% and fewer complications than surgery. The procedure usually takes less than an hour, and the incision site is usually small enough that stitches aren’t required. After the procedure, you should expect some bruising and may be encouraged to walk for 30–60 minutes. You should also avoid strenuous activities like jogging or weight lifting, and sitting or standing for long periods of time, until your doctor says it’s okay. Most people can return to work and normal activities after a couple of days.
Before your procedure, your doctor may ask you to stop taking blood thinners like aspirin, so it’s important to understand exactly what they want you to do.
Venaseal
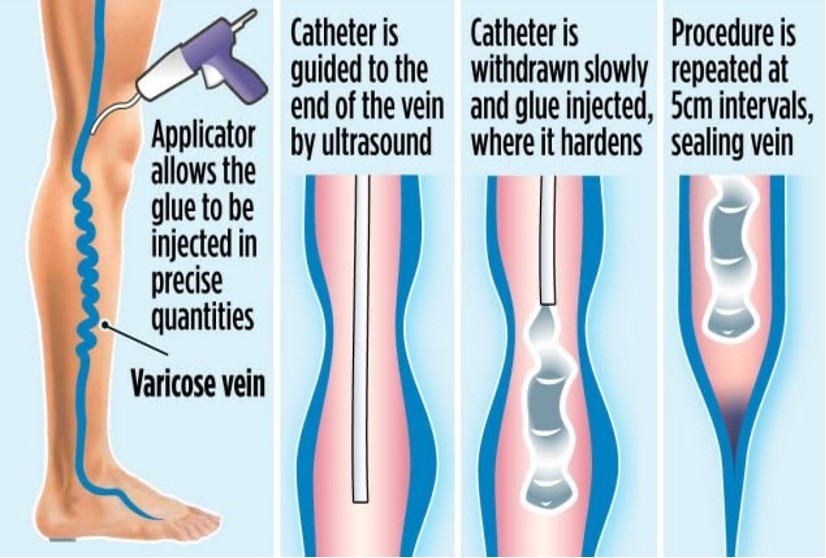
VenaSeal ablation is a minimally invasive procedure that uses medical glue to close damaged veins and improve varicose veins. The procedure can help relieve symptoms associated with damaged veins, such as leg pain, swelling, and fatigue, and can also gradually fade varicose veins.
During the procedure, a vein expert uses ultrasound guidance to deliver a small amount of the glue directly into the affected vein through a small catheter. The glue holds the vein walls together, stopping blood flow to the damaged area and redirecting it to healthy veins. Over time, the body absorbs the inactive veins, and they disappear.
VenaSeal ablation is a day procedure that takes about 45–60 minutes, but patients typically spend 4–6 hours at the facility. It’s considered a comfortable procedure with a quick recovery, and patients can usually return to their normal activities right after. Some people may experience minor bruising and swelling at the injection site, but most recover with minimal discomfort.
VenaSeal ablation has several advantages over other treatments, including:
However, there are also some potential disadvantages to consider, including:
Sclerotherapy
Sclerotherapy is a medical procedure that involves injecting a chemical solution into veins to treat varicose and spider veins. The solution irritates the vein lining, causing it to swell, stick together, and form a scar that closes off the vein. This can improve the appearance of the veins and relieve symptoms like aching, swelling, burning, and cramping. The vein usually fades within a few weeks.
After treatment, patients may be advised to:
Most patients need two to four treatment sessions to see near-complete results, but complete elimination of the veins isn’t guaranteed
Stab phlebectomy
A stab phlebectomy, also known as microphlebectomy, ambulatory phlebectomy, or stab avulsion, is a minimally invasive procedure that removes varicose veins from the surface of the legs:
The procedure usually takes about an hour and patients typically report little pain. After the procedure, patients can walk and usually resume normal activities within 1–2 days. They may be advised to wear compression bandages or stockings for a period of time.
Stab phlebectomies are safe and effective, but there is a small risk of temporary side effects, such as:
Stab phlebectomy has been used since the 1800s and is often used for cosmetic surgery, symptomatic varicose veins, or larger veins that can’t be treated with newer technologies.
Wound Care
Vascular Institute of Michigan can diagnose and treat patients with ischemic, venous, diabetic and small vessel ulcers.
Chronic wounds develop from various aetiologies including pressure, diabetes, venous pathology, and surgery. A pressure ulcer is defined as a localized injury to the skin and or underlying tissue occurring most often over a bony prominence and caused, alone or in combination, by pressure, shear, or friction. Up to three fifths of venous leg ulcers are due to venous aetiology.
Up to 65% of those afflicted by chronic leg ulcers report experiencing decreased quality of life, restricted mobility, anxiety, depression, and/or severe or continuous pain.